RCM Outsourcing Improves Cost to Collect for Healthcare Organizations
It’s a dilemma all healthcare organizations and hospitals routinely face — how to maintain profitability and deliver high-quality patient care. For some organizations, the high cost and complexity of managing the revenue cycle can derail efforts to achieve revenues that outpace expenditures.
Cost to collect — the total amount hospitals spend on revenue cycle functions, including expenses related to staff, salaries, and technology — is a key performance indicator that healthcare organizations should pay close attention to when tracking revenue cycle management costs. These expenses can mount quickly and adversely affect an organization’s bottom line.
The industry standard for cost to collect is around 3 to 4%, but this figure can vary based on the size and type of healthcare setting.1 A lower cost to collect metric usually indicates a healthcare organization takes an optimized approach to the revenue cycle, which can lead to increased profitability. Though the formula for calculating the cost to collect is a simple one (total revenue cycle costs divided by the total patient service cash collected), determining how to mitigate those costs is not quite so straightforward. This white paper discusses the cost to collect challenges healthcare organizations face and the benefits of outsourcing revenue cycle functions to enhance profit margins.
Ongoing Revenue Cycle Challenges
The healthcare revenue cycle process is a complicated maze comprised of internal and external stakeholders, coding and billing systems, and industry regulations. To receive compensation for services rendered, healthcare organizations and hospitals must weave through a labyrinth of documentation, payer guidelines, and compliance rules, all while dealing with the issue of healthcare technology interoperability and data security. These mission-critical RCM functions often strain administrative workloads and increase operational costs.
Adding to these budgetary pressures is healthcare organizations’ struggle to obtain payment from patients who are feeling the financial weight of higher deductibles and copays, another factor adversely impacting margins. According to the 2022 Uncompensated Care Fact Sheet published by the American Hospital Association, since 2000, hospitals of all types have provided almost $745 billion in uncompensated care to their patients.2 In 2022, the American Hospital Association found more than half of U.S. hospitals had a negative margin.3 And a Deloitte survey of health care C-suite executives showed only 3% have a positive outlook on the industry for 2024 compared to 15% last year.4
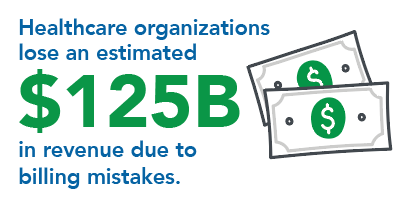 Not only are hospitals experiencing revenue recovery losses from uncompensated care, but they have also seen a reduction in reimbursement rates from private payers and government-funded health insurance programs. The financial fallout from unpaid care and lower payer rates has caused several healthcare organizations to close medical departments or end services at facilities to stay open. Moreover, billing errors due to manual coding processes, poor documentation, and convoluted billing regulations can cause delayed payments or even denials. Healthcare organizations lose an estimated $125 billion in revenue due to billing mistakes alone.5 The task of appealing denied claims is labor and time-intensive, which further increases administrative costs and decreases cash flow.
Not only are hospitals experiencing revenue recovery losses from uncompensated care, but they have also seen a reduction in reimbursement rates from private payers and government-funded health insurance programs. The financial fallout from unpaid care and lower payer rates has caused several healthcare organizations to close medical departments or end services at facilities to stay open. Moreover, billing errors due to manual coding processes, poor documentation, and convoluted billing regulations can cause delayed payments or even denials. Healthcare organizations lose an estimated $125 billion in revenue due to billing mistakes alone.5 The task of appealing denied claims is labor and time-intensive, which further increases administrative costs and decreases cash flow.
To further complicate matters, the aftermath of Covid has left many healthcare organizations dealing with deficiencies in RCM staff, expertise, and technology infrastructure. U.S. hospitals and health systems face significant increases in the costs required to care for patients and communities putting their financial stability at risk. These factors include historic inflation driving up the cost of medical supplies and equipment, and critical workforce shortages, and sustained demand for hospital care with patients coming to the hospital sicker and staying longer has exacerbated these challenges.3
It is becoming increasingly more challenging for hospitals to keep pace with evolving regulatory requirements, industry best practices, and technological advancements. As such, these organizations lack the ability to curtail revenue leakage and control costs. To achieve and maintain profitability, healthcare organizations have a business imperative to maximize collections and mitigate financial losses by optimizing RCM processes.
Outsourcing RCM to Reduce the Cost to Collect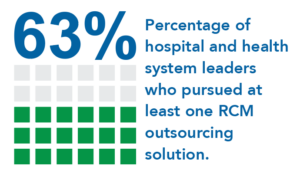
Organizations that have shrinking revenue cycle margins should consider automating processes and partnering with an experienced RCM vendor. Although many healthcare organizations and hospitals are wisely conducting assessments to identify shortfalls in their current RCM approach, often their already strained budgets make it difficult to implement the needed process improvements internally. This is where outsourcing RCM processes can add value to an organization. A 2022 Kaufman Hall State of Healthcare Performance Improvement report revealed that up to 61% of providers plan to outsource RCM tasks in the future. The report also showed that 63% of hospital and health system leaders surveyed had pursued at least one outsourcing solution with revenue cycle functions being at the top of the list (27%).6
Healthcare organizations that partner with a proven RCM vendor may be spared the expense of upgrading or replacing legacy systems because the vendor has already invested in powerful automation technologies. These include billing software, data analytics tools, robust security, and cloud-based platforms that offer scalability and flexibility for adapting to industry changes. Automating routine RCM tasks streamlines workflows and enables hospitals to eliminate the need for internal staffing, and training, which reduces overhead expenses, increases cash flow, and enhances operational efficiency.
The revenue cycle encompasses complex processes and requires specialized expertise for hospitals to increase their capture rate and revenue recovery. This is one key reason many healthcare organizations are choosing to outsource this mission-critical function. Once a decision has been made to outsource RCM, it is important to select an RCM vendor that has proven healthcare experience and expertise.
Conclusion
Healthcare organizations continue to face financial pressures in the current environment, and the challenges of effectively managing the revenue cycle can impact their profitability and sustainability. The good news is that hospitals can overcome shrinking margins by partnering with an experienced and results-oriented RCM vendor. The outsourcing of revenue cycle functions has become a business imperative that will enable healthcare organizations to increase cash flow and maintain financial viability. Using specialized expertise, technology, and strategic insights, a proven RCM partner enables healthcare organizations to streamline revenue cycle operations, improve billing accuracy, and enhance compliance, which ultimately helps drive financial performance and supports the delivery of high-quality patient care.
About Elevate Patient Financial Solutions®
Elevate Patient Financial Solutions® is a trusted partner that delivers superior RCM solutions to hospitals, health systems, and healthcare providers nationwide. For more than 40 years, ElevatePFS has been developing and continually refining their best-in-class services and innovative, specialized technology to address the most complex challenges of the revenue cycle.
ElevatePFS has carefully built teams with unmatched industry experience and service-specific expertise, and their commitment is to deliver on their promises, seek continuous improvement and the pursuit of excellence to deliver elevated results for their clients.
ElevatePFS services include Eligibility & Disability Advocacy, Self-Pay, Third Party Liability, Workers’ Compensation, Veterans Administration, COB Denials, Out-of-State Eligibility, and a range of A/R Services, including High and Low Balance A/R projects, Zero Balance Payment Recovery, Legacy Receivables and Extended Business Office engagements.
References
- https://revcycleintelligence.com/news/automating-revenue-cycle-operations-can-reduce-cost-to-collect
- https://www.aha.org/system/files/media/file/2020/01/2020-Uncompensated-Care-Fact-Sheet.pdf
- https://www.aha.org/system/files/media/file/2023/04/Cost-of-Caring-2023-The-Financial-Stability-of-Americas-Hospitals-and-Health-Systems-Is-at-Risk.pdf
- https://www2.deloitte.com/us/en/blog/health-care-blog/2023/outlook-for-health-care.html
- https://www.thebusinessresearchcompany.com/report/medical-billing-outsourcing-global-market-report#:~:text=It%20is%20also%20estimated%20that,the%20medical%20billing%20outsourcing%20market.
- https://www.kaufmanhall.com/sites/default/files/2022-10/2022-State-Healthcare-Performance-Improvement.pdf
