Eligibility Partnership Case Study
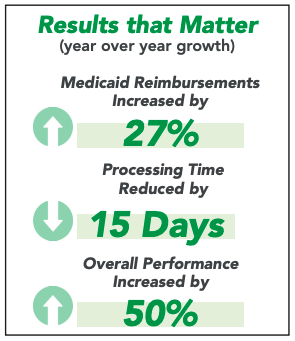
Health System Partners with RCM Vendor to Streamline Medicaid Program and Significantly Increase Reimbursements
In early 2020, a large non-profit health system on the East Coast decided that its Pending Medicaid program could be more effective. The program was fragmented, with siloed responsibility. Many areas of the process needed additional oversight, and internal staff needed help with delays and confusion that resulted in denials, and lost revenue with self-pay accounts, Medicaid, and other potential reimbursements. The health system realized that as its uninsured patient population grew, it was necessary to augment, streamline, and standardize their processes by partnering with a trusted revenue cycle vendor that could increase conversions and reimbursement, and while providing compassionate financial advocacy for their patients. Upon close examination, the system estimated these process issues led to a loss of $13 million in potential revenue. The health system partnered with Elevate Patient Financial Solutions® and the company's Eligibility & Enrollment solution successfully helped the client overhaul their Pending Medicaid process.
Click the button below to download the full case study and learn how ElevatePFS identified program issues resulting from the pandemic, resolving a backlog of more than $15 million in charges.