Eligibility Head-to-head Analysis Case Study
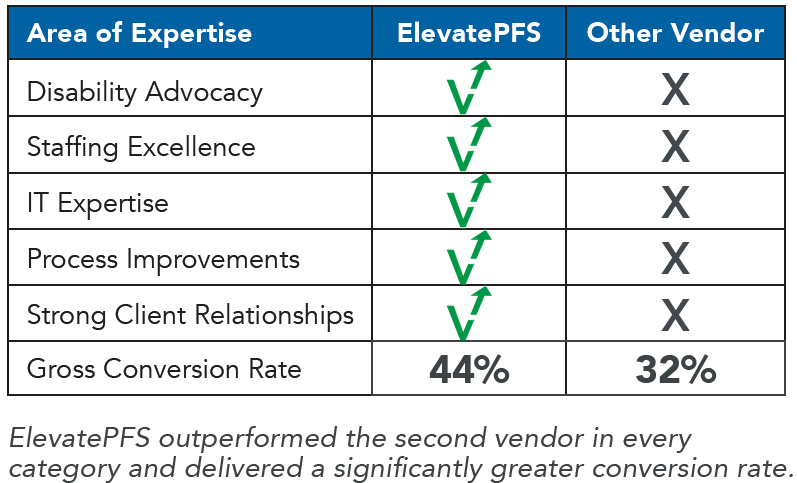
ElevatePFS Outperforms Competitor in Head-to-head Analysis
After a solid 14-year relationship, a large not-for-profit healthcare organization with hospitals and health providers in the South wanted to reaffirm it had the best revenue cycle management partner in Elevate Patient Financial Solutions® for its eligibility and enrollment needs. The organization wanted to make sure they were being good stewards of their resources and to improve their staffing and collaboration with their departments, including their case management team. In a head-to-head analysis, the organization gave half of their eligibility accounts to a second revenue cycle vendor to see if they could do a better job of improving their processes and to see if ElevatePFS could still provide exceptional Eligibility & Enrollment results for them.
Click the button below to download the full case study and learn how ElevatePFS won back all the client's eligibility business and achieved a gross conversion rate of 44% — 12% more than the second vendor.