Compilation Eligibility Case Study
Top Rated Eligibility Services Expert Delivers Exceptional Performance, Improves Patient Experience
The number of people without medical insurance is increasing and many are unaware that they may qualify for government assistance programs such as Medicaid. Enrolling in these programs can be confusing for patients and often involves the time-consuming task of filling out a lot of paperwork. The process of screening patients for eligibility for federal, state, and local programs and helping with enrollment requires a high level of expertise and time to devote to the follow-up process. As costs rise and workforce challenges continue, providers look to outsource Eligibility & Enrollment services to alleviate the financial burden of medical bills for their patients.
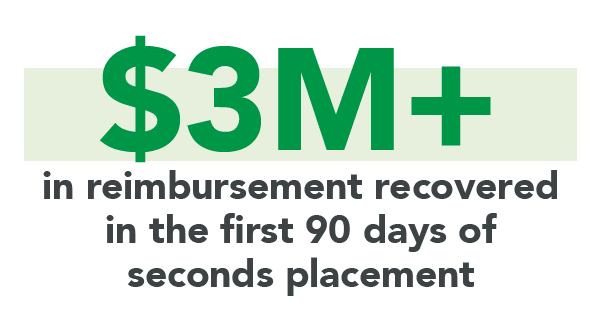
Click the button below to download the full case study and learn how Elevate Patient Financial Solutions® outperformed several competitors, achieving $3 million in reimbursement in the first 90 days of seconds placement for one client and an increase of 30% in revenue recovery for another.